Back Surgery Part 2 – How Back and Neck Surgery can Damage the Spine
In the first part of this series, I described the pros and cons of back surgery, my personal experience of cancelling two different back surgeries, and my experience with helping clients to avoid surgery.
I also discussed the importance of seeing surgery as only a last resort, reasons why back surgery often “fails”, and who is ultimately responsible for one’s back and neck health.
There are several types of back and neck surgery, such as discectomy, where a spinal disc that may be herniated and pushing on a nerve root or the spinal cord is removed, and fusion, where two or more spinal vertebrae are “fused” together, which also requires removal of the disc.
Both of these surgeries often require an extended recovery period. Discectomy can have several severe consequences, and fusion often results in adjacent segment disease, since other structures have to over-compensate for the lack of function and mobility and then they become unstable.
In this article, I will discuss the problems associated with two other common back and neck surgeries: wide laminectomy and open door laminoplasty.
Regenexx
In my research on back and neck surgery, I’ve often come across the work of Dr. Chris Centeno, who is board certified in Physical Medicine and Rehabilitation. According to Dr. Centeno, “There are certain people that do need surgery, but in my experience that’s maybe one in ten to one in five patients that currently get it.”
In other words, many people that are prescribed surgery might have much more success with other less-invasive techniques, such as physical therapy, therapeutic massage, and specific targeted injections.
Dr. Centeno’s primary clinic is in Colorado, and he has trained specialists located around the country in highly successful techniques to restore function to spinal joints and other joints in the body without using common, invasive surgical methods.
His company is called Regenexx, which has sponsored many well-designed studies on the effects of Interventional Orthopedics, which includes a class of techniques that Dr. Centeno helped pioneer. The images in this article come from a case study on Dr. Centeno’s website, https://regenexx.com/.
I and several people I know well have experienced the work of Dr. Keley Booth, who is a pain management specialist in Oklahoma City, and who was trained at Regenexx. I have been greatly impressed by Dr. Keley’s diagnostic methods, his willingness to take the time to explain and educate, and the success of his treatments.
A Case Study
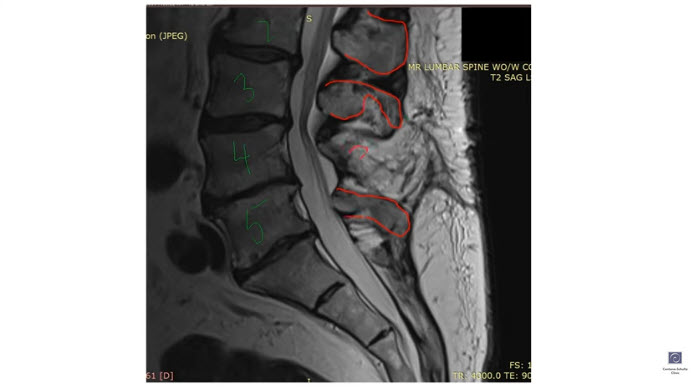
Dr. Centeno describes one elderly male patient that came to him with several severe back and neck pathologies. Ten years earlier, he had painful leg symptoms, and his doctor prescribed and performed a wide laminectomy surgery. Shortly after the surgery, the pain returned.
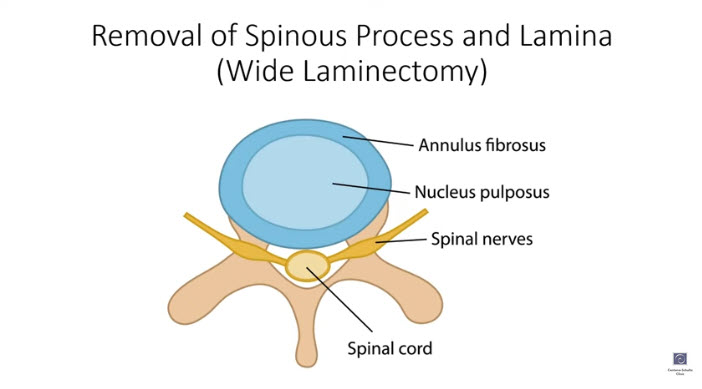
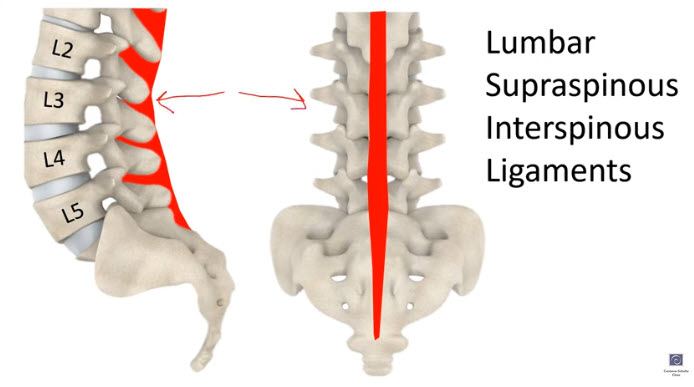
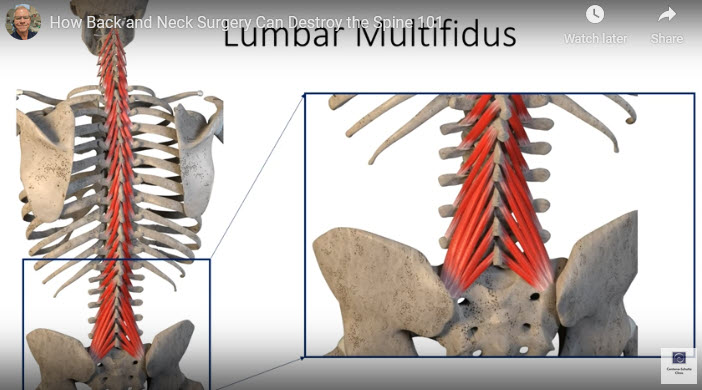
With this wide laminectomy, the surgeon removed the L4 spinous process and part of the lamina (vertebral bone) to open up the spinal canal. With the L4 spinous process gone, the spinous ligaments were no longer attached from L3 down to L5. Also, the multifidus muscle was no longer attached, causing it to essentially “die”.
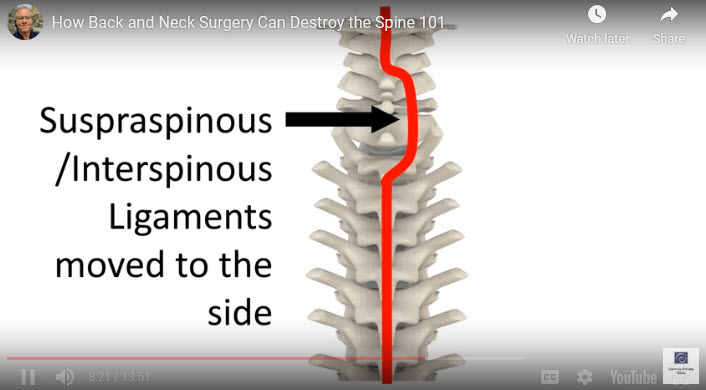
These spinal ligaments and multifidus muscles are important stabilizers for the low back. Dr. Centeno says that the lumbar supraspinous and interspinous ligaments are “critical stabilizing ligaments that allow the lumbar spine to remain stable when you do things like bend forward”.
He also describes the multifidus muscles as “absolutely critical – everything you do requires these stabilizing muscles”. Without them the spine becomes unstable, potentially irritating spinal nerves and causing symptoms like leg pain.
That’s exactly what happened to this patient. His leg pain returned, and the post-surgery MRI showed why the pain returned. The surgery had essentially destabilized the supportive structures in that part of his lumbar spine, leading to more back and leg pain.
If back surgery doesn’t help, try, try again…
The surgeon did not recognize that the surgery itself was a major trigger of the patient’s leg pain recurrence. Instead, he decided to look at the neck to see if it was the culprit.
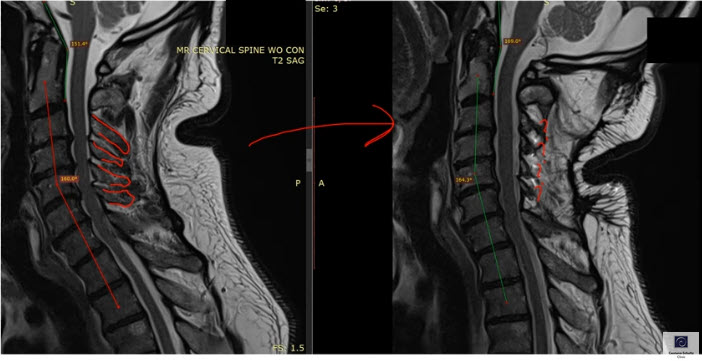
The MRI on the cervical spine showed some areas of stenosis, which is a narrowing of the spinal canal that can produce pressure on the spinal cord or nerve roots. The doctor decided that this was the cause of the leg pain, though he didn’t do any testing to confirm that, such as a spinal epidural to see if leg pain went away.
The surgeon went back to work and did a C3-C6 open door laminoplasty. This procedure involves cutting into the lamina and swinging the spinous process to the side. The spinous ligaments get moved over, as well. And the surgeon has to cut through the multifidus on one side in order to get to lamina.
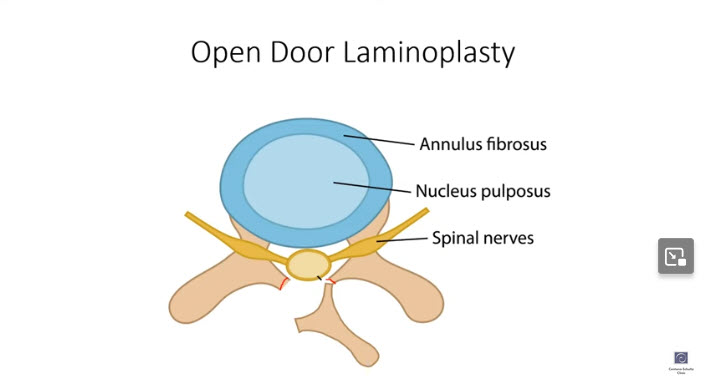
Meanwhile, the structures on the Other side of the spine get scrunched up by the spinous process. In this case, everything from C3-C6 was pushed over to one side of the spine, so that the ligaments and multifidi did not perform their stabilizing function properly anymore.
As a result, the spinous ligament “suspension bridge” of the neck was now damaged, and the stabilizing spinous muscles were also damaged. In addition, the patient’s neck curve lost its natural curve and got noticeably straighter because of the loss of ligament stabilization of the neck.
Unfortunately, this operation did not alleviate the patient’s leg pain. Instead, it caused new neck and head symptoms, and he couldn’t hold his head up comfortably anymore. That’s not what one hopes for when going in for back surgery!
Word to the Wise re Back Surgery
With the damaging effects of these surgical procedures, all this patient could do now is multiple fusions and hope for the best. As Dr. Centeno explains, if he had received some of the less invasive orthobiologic procedures early on, he might have avoided years of pain and suffering.
These orthobiologic procedures include more specific diagnosis, targeted platelet-rich plasma injections, prolotherapy, and targeted bone marrow stem cell injections (which is very different from common stem cell procedures). Dr. Centeno and the doctors he has trained have had ample success with these techniques in reducing pain and increasing mobility and quality of life – without surgery.
I recommend that you watch Dr. Centeno’s video on this case study at his Regenexx website. While you’re there, subscribe to his blog. He always has topics related to back surgery and other areas of interest to massage therapists and other practitioners.
If you or your client or someone else you know is prescribed back or neck surgery, it’s always best to get a second opinion, start with good physical therapy and therapeutic massage, and research potentially helpful ways to avoid going under the knife.
If you’re interested in learning successful therapeutic massage techniques, view the Ray of Light Training Online CE Courses and DVDs here:
https://roltraining.com/product-category/courses/
Stay well, John
John Joseph Ray
Ray of Light Training
John is a Board Approved Continuing Education Provider through the NCBTMB
Member of the Fascia Research Society
